When people eat sugars and starches, the body breaks them down into glucose with the help of insulin, the hormone that gets glucose from the bloodstream into the cells of the body to be used as energy. However, for some people with Type 2 diabetes, this process cannot happen without manually giving insulin subcutaneously, since the pancreas, (the organ that produces insulin) stops doing so. Insulin must be injected and infused into the layers of fat under the skin. There are different kinds of insulin delivery methods, each with pros and cons, and it is up to the person with diabetes and his or her doctor to decide what will work best.
Syringes

How it works:
- Before anything, it is important to wash your hands and clean the skin with alcohol.
- You’ll first need to uncap the needle of the syringe.
- Pull the plunger to fill the syringe with air.
- Insert the needle of the syringe into the vial of insulin.
- Draw the plunger until the appropriate dose of insulin is inside the syringe barrel.
- Holding the syringe upright, tap the syringe to release any air bubbles that may have collected in the barrel.
- Next, insert the needle into the skin using your index finger or thumb and push the plunger down until all the insulin has emptied from the barrel.
- Re-cap needle and dispose of in a secure sharps container.
How long it lasts:
For one-time use and should be disposed of immediately following use into a sharps container
Cost:
$10-15 per box of 100. Price may vary based on insurance coverage.
Pros:
You don’t have the burden of a device attached to you.
Cons:
You have to carry syringe supplies and vials of insulin with you and make sure you don’t forget any of the steps involved in drawing up a dose of insulin. (A vial of insulin at room temperature should only be used for 28 days from opening, and must be disposed of after this time, even if there is insulin leftover.) This can result in wasted insulin.
Pens
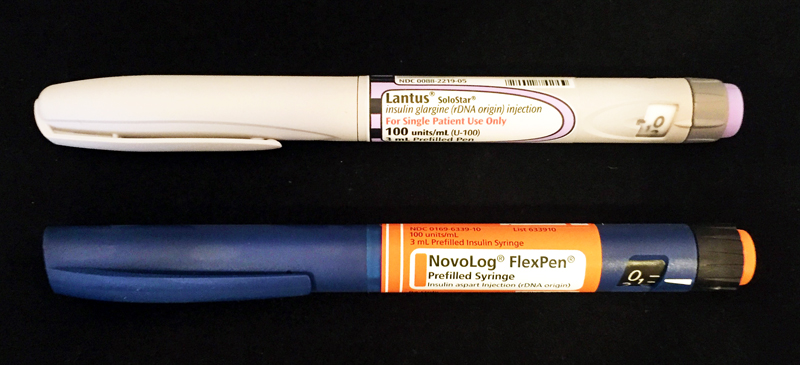
How it works:
- Prepare and clean the skin with alcohol wipes.
- Uncap the pen.
- Attach the pen needle.
- Dial-up the dose using the dial on the end of the pen opposite the needle.
- If using a pen for the first time, prepare the pen by first drawing in a very small dose of insulin and then pushing it into the air.
- Insert the needle into the skin and push in the end to administer insulin.
- When done, remove the pen needle and dispose of it in a secure sharps container.
How long it lasts:
Some pens are disposable, others have replaceable cartridges of insulin that can be inserted into the pen. Once opened and stored at room temperature a pen is good for 28 days before it must be replaced.
Cost:
Varies drastically depending on the insulin you are using, the pen brand and your insurance; $20-70 per box of 100 disposable needles (costs varies depending on the gauge of the needle).
Pros:
Their small size and likeness to ink pens make insulin pens a convenient and discreet way of carrying insulin. They’re often less painful than syringes because of smaller needles.
Cons:
The pen needs to remain in the skin slightly longer than a traditional syringe injection, about 5 seconds after the plunger has been released. Pens can also be easy to lose or forget.
Pod Therapy

How it works:
- Pod therapy by Insulet’s Omnipod DASH Insulin Management System is a tubeless, wearable, waterproof insulin pump that can hold up to 200 units of insulin and delivers 72 hours of continuous insulin therapy through customizable basal rates and bolus amounts. Basal dosages keep your blood sugar stable over time and “bolus” insulin dosages are given for meals or to correct high blood sugar.
- Omnipod DASH users get a personal diabetes manager (PDM) to wirelessly control the Pod.
- Complimentary iPhone widgets give users the ability to see their CGM data and insulin delivery information together on a single screen.
- Two iOS mobile apps — Omnipod DISPLAY and Omnipod VIEW — allows users to see their PDM information on their smartphone and share therapy status with up to 12 friends/family members.
- Users get access to a CalorieKing food library with carbohydrate content for over 80,000 foods.
How long it lasts:
The pump holds a small cartridge of insulin that usually needs to be replaced every 3 days to prevent bruising, insulin buildup, scar tissue, and possible infections.
Cost:
Omnipod can be as low as a $20 co-pay through the pharmacy, which is another benefit of this product.
Pros:
- Customizable basal insulin profile and bolus calculator. This means you can customize how much insulin you need throughout the day based on insulin sensitivity. With the bolus calculator, you can determine how much insulin you need based on the number of carbs in your meal.
- While traditional pumps have infusion set tubing that connects the pump to the body, however, the Omnipod Insulin Delivery System, does not have tubing and adheres to the body anywhere an injection would be administered.
- With the Omnipod Delivery System’s auto cannula insertion, you don’t need to see or handle a needle when changing your pump site.
- More accurate insulin injections. Insulin can also be injected in smaller dose increments.
- Improved glucose management compared with injections.
- Easier to dose insulin for meals and exercise.
- Decreased risk of hypoglycemia and diabetes-related complications.
- Can adjust insulin dosages as you see fit.
Cons
- The idea of wearing a device 24/7 can be off-putting for some people.
- There is always the possibility of the pump malfunctioning.
Insulin Pumps

How it works:
- Similar to the section above, pumps are small, computerized devices that deliver fast or short-acting insulin over a 24 to 72 hour period through a catheter placed under the skin. Traditional insulin pumps have infusion set tubes that connect from the pump to a part of your body.
- Many pumps have features to ensure effective insulin delivery + glucose management such as carb-to-insulin ratio, correction factors, target BG levels, and insulin sensitivity.
- The pump will then help you calculate how much insulin to administer based on your blood sugar or carb count. However, you can also “bolus” manually without the use of the pump calculator.
- Some pumps are now integrated with continuous glucose monitoring (CGM) technology, which tracks your blood glucose on an ongoing basis.
How long it lasts:
Just like in the previous section, you should change your infusion set and pump set every 2 to 3 days. To prevent bruising, scar tissue, and infections, please follow your manufacturer’s recommendation on when to change your pump site and infusion set. Depending on which brand you use, your pump may also automatically remind you when to do so. The actual pump devices typically last 4-5 years, but many will still work after their warranty has expired.
Cost:
$4,500-6,500 without insurance. Please check with your health insurance company to determine the final cost for your plan.
Pros:
- You don’t have to individually stick yourself with a needle every time you need to inject insulin, instead, you only have to use a needle once every three days to insert the catheter.
- Pumps deliver insulin more accurately than injections and can be injected in smaller dose increments.
- Improved glucose management compared with injections.
- Easier to dose insulin for meals and exercise.
- Decreased risk of hypoglycemia and diabetes-related complications.
- Can adjust insulin dosages as you see fit.
Cons
- Pumps can be expensive, even with insurance.
- The idea of wearing a device 24/7 can be off-putting for some people, especially if it is a pump with tubing.
- Pump sites can be ripped out accidentally and get snagged onto objects. There is also the possibility of the pump malfunctioning.
Inhaled insulin

How it works:
- Inhaled insulin is used as a mealtime insulin, designed specifically to lower blood sugar spikes that can happen after you eat.
- It works faster than traditional injected insulins.
- Using an inhaler similar to those used for asthma, you breathe a fine insulin powder into your lungs.
- The insulin then enters your blood through small blood vessels.
How long it lasts:
Once opened, the inhalers can be used for up to 15 days.
Cost:
Afrezza, currently the only inhaled insulin approved by the Food and Drug Administration, may be covered by your insurance. Check with your provider for exact costs. Afrezza’s website offers an option to sign up for a $0 co-pay on your first prescription. There is also a saving program.
Pros:
- No invasive needle injections mean no pain
- Because it peaks in 30 minutes, you don’t have to wait as long to eat and are less likely to stack insulin in anticipation
- A recent STAT study also cited the benefits of reduced incidences of hypoglycemia
Cons:
- You’ll still need to take long-acting insulin to monitor your blood sugar
- Side effects may include a cough and throat irritation
- Not recommended for patients with asthma or who smoke
- It is not known if Afrezza is safe and effective in children under 18
Disposable Insulin Devices (V-Go)

How it works:
- V-Go is a portable, tubeless, disposable insulin delivery system (like a mini pump)
- Fill your V-Go with fast-acting insulin such as Humalog or Novolog.
- V-Go can be worn in a variety of locations on your body, and the location can be changed based on your preference or clothing choice each day:
- Just clean your preferred area, remove the adhesive, and apply V-Go.
- Then press the start button to start the flow of insulin through a small, flexible needle.
- Click buttons on the device to administer more insulin around mealtime.
- V-Go is for people with Type 2 diabetes who require 20, 30, or 40 units per day.
How long it lasts
- 24-hours
Cost
- Around $250 for a 30-day supply
Pros
- No need to carry supplies, such as pens, needles, vials, and syringes
- Discrete
- Does not require batteries
Cons
- You have to change it daily